Definitions and modalities are expanding but in general, there are three types of virtual care: synchronous, asynchronous or “store-and-forward,” and remote patient monitoring (RPM). The COVID-19 pandemic accelerated adoption and utilization of all types at record pace, including the latter.
Patients had to stay away from many clinical settings during the pandemic lockdown so clinicians turned to RPM to monitor their patients’ care from home. A study by MSI International found that more than 23.4 million patients used RPM to monitor their health in 2020, up from 7 million in 2016. That number is expected to increase by 28% to 30 million patients by 2024, or 11.2% of the US population.
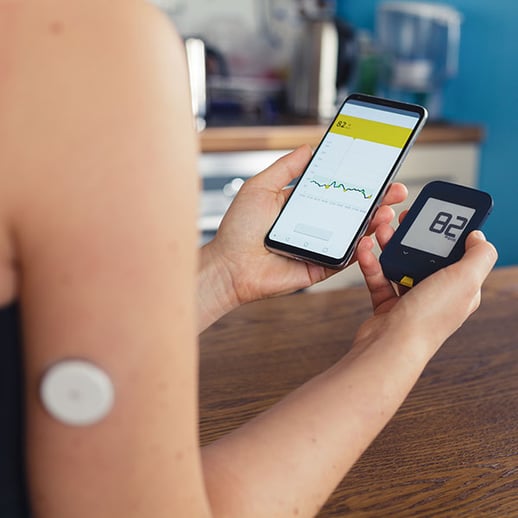
As with other telehealth services, consumers have embraced RPM. A survey conducted in May 2021 found that 65 to 70% of patients would partner with their provider and use RPM to monitor blood pressure, heart rate, blood sugar and blood oxygen levels. A larger survey from June 2020 found 75% of chronic disease patients and caregivers said they would be willing to use an RPM tool to assist with care.
Is this finally the tipping point for telehealth? Recently in Forbes, Stephen Wunker identified factors that make this the “inflection point” for RPM. They apply to telehealth in general as well.
Patient habit: Patients are more receptive to remote consultations after COVID-19, have more confidence in telehealth, and substantial marketing by tech vendors has normalized wearables and interaction with digital health gadgets.
Physician habit and practice workflow: Previously, devices would collect data but physicians, clinicians and staff would not necessarily download it in a timely manner, use it consistently, or integrate it into care plans. When most patient interactions were conducted remotely, practitioners developed systems to conduct virtual visits, monitor patients at home, collect data, synthesize data and visits, and incorporate all to manage patient care. From necessity comes adoption of new modalities, development of new processes, and before you know it, what was once new is now an integral part of patient care.
Reimbursement: COVID-19 prompted all payers to reimburse for telehealth. Previously, we examined whether expanded payment will remain.
EMRs: While true EMR interoperability still remains far from seamless or painless, there is slow improvement meaning less friction for physicians to synchronize data from telehealth and digital products into EMRs.
Technology: Telehealth platforms, digital products, IT systems are all evolving and improving at lightning speed making them easier to use, more convenient for patients, and more functional and effective for clinicians. Most significantly, digital tools are improving outcomes.
Providers using RPM and other home monitoring systems report reduced hospital readmission penalties. By equipping patients with tablets and RPM equipment, for example, the University of Pittsburgh Medical Center reduced the risk of hospital readmission by 76% while having patient satisfaction scores over 90%.
It is obvious that telehealth and RPM are and should continue to be essential components in providing comprehensive, more coordinated, patient-centered care and that telehealth will help providers improve quality. Let us hope lawmakers, policymakers and payers find it obvious as well.
